Ayushman Bharat Yojana Grievance Redressal Guideline
1. Guideline for Grievance Redressal
Grievance Department has to be manned by dedicated resources to address the grievances
from time to time as per the instructions of the NHA. The District authorities shall act as a
frontline for the redressal of Beneficiaries’/ Providers/ other Stakeholder’s grievances. The
District authorities shall also attempt to solve the grievance at their end. The grievances
so recorded shall be numbered consecutively and the Beneficiaries / Providers shall be
provided with the number assigned to the grievance. The District authorities shall
provide the Beneficiaries / Provider with details of the follow-up action taken as
regards the grievance as and when the Beneficiaries require it to do so. The District
authorities shall also record the information in pre-agreed format of any complaint /
grievance received by oral, written or any other form of communication.
Under the Grievance Redressal Mechanism of PMRSSM, following set of three tier Grievance
Redressal Committees have been set up to attend to the grievances of various stakeholders
at different levels:
District Grievance Redressal Committee (DGRC)
The District Grievance Redressal Committee (DGRC) will be constituted by the State Health
Agency (SHA) in each district within 15 days of signing of MoU with the Insurance Company.
The District Magistrate or an officer of the rank of Addl. District Magistrate, who
shall be the Chairperson of the DGRC.
The CMO/ CMOH/ DM&HO/ DHO or equivalent rank officer shall be the
Convenor of the DGRC.
Representatives from the district level offices of the Departments of Rural
Development.
The District Coordinator of the Insurer.
The District Grievance Nodal Officer (DGNO)
The DGRC may invite other experts for their inputs for specific cases.
Note: DGNO shall try to resolve the complaint by forwarding the same to Action Taking
Authority (ATA). If the complaint is not resolved or comments are not received over the
same within 15 days of the complaint, then the matter may be referred to DGRC.
State Grievance Redressal Committee (SGRC)
The State Grievance Redressal Committee (SGRC) will be constituted by the State Health
Agency within 15 days of signing of MoU with the Central Government.
CEO of State Health Authority / State Nodal Agency shall be the Chairperson of
the SGRC.
Representatives of the Departments of Rural Development, Women & Child
Development, Labour, Tribal Welfare.
Director Health Services.
Medical Superintendent of the leading state level government hospital.
The State Grievance Nodal Officer (SGNO) of the SHA shall be the Convenor of
SGRC.
The SGRC may invite other experts for their inputs on specific cases.
Note: In case of any grievance between SHA and Insurance Company, SGRC will be chaired
by the Secretary of Department of Health & Family Welfare of the State. If any party is not
agreed with the decision of DGRC, then they may approach the SGRC against the decision
of DGRC.
National Grievance Redressal Committee (NGRC)
The NGRC shall be formed by the MoHFW, GoI at the National level. The constitution of the
NGRC shall be determined by the MoHFW in accordance with the Scheme Guidelines from
time to time.
Proposed members for NGRC are:
1. CEO of National Health Agency (NHA) – Chairperson
2. JS , Ministry of Health & Family Welfare- Member
3. Additional CEO of National Health Agency (NHA)- Member Convenor
4. Executive Director, IEC, Capacity Building and Grievance Redressal
5. NGRC can also invite other experts/ officers for their inputs in specific cases
CEO (NHA) may designate Addl. CEO (NHA) to chair the NGRC.
Investigation authority for investigation of the grievance may be assigned to Regional
Director- CGHS/Director Health Services/ Mission director NHM of the State/UT
concerned.
NGRC will consider:
a. Appeal by the stakeholders against the decisions of the State Grievance Redressal
Committees (SGRCs)
b. Also, the petition of any stakeholder aggrieved with the action or the decision of the
State Health Agency / State Government
c. Review of State-wise performance based monthly report for monitoring, evaluation
and make suggestions for improvement in the Scheme as well as evaluation
methodology
d. Any other reference on which report of NGRC is specifically sought by the
Competent Authority.
The Meetings of the NGRC will be convened as per the cases received with it for
consideration or as per the convenience of the Chairman, NGRC.
1.1. Grievance Settlement of Stakeholders
If any stakeholder has a grievance against another one during the subsistence of the
policy period or thereafter, in connection with the validity, interpretation,
implementation or alleged breach of any provision of the scheme, it will be settled in
the following way by the Grievance Committee:
A. Grievance of a Beneficiary
i) Grievance against insurance company, hospital, their representatives or any
functionary
If a beneficiary has a grievance on issues relating to entitlement, or any other
PMRSSM related issue against Insurance Company, hospital, their representatives or
any functionary, the beneficiary will approach DGRC. The DGRC shall take a decision
within 30 days of receiving the complaint.
If either of the parties is not satisfied with the decision, they can appeal to the SGRC
within 30 days of the decision of the DGRC. The SGRC shall take a decision on the
appeal within 30 days of receiving the appeal. The decision of the SGRC on such
issues will be final.
Note: In case of any grievance from beneficiary related to hospitalisation of beneficiary
(service related issue of the beneficiary) the timelines for DGRC to take decision is within
24 hours from the receiving of the grievance.
ii) Grievance against district authorities
If the beneficiary has a grievance against the District Authorities or an agency of the
State Government, it can approach the SGRC for resolution. The SGRC shall take a
decision on the matter within 30 days of the receipt of the grievance. The decision of
SGRC shall be final.
B. GRIEVANCE OF A HEALTH CARE PROVIDER
i) Grievance against beneficiary, insurance company, their representatives or
any other functionary
If a Health Care Provider has any grievance with respect to beneficiary, Insurance
Company, their representatives or any other functionary, the Health Care
Provider will approach the DGRC. The DGRC should be able to reach a decision
within 30 days of receiving the complaint.
Step I- If either of the parties is not satisfied with the decision, they can go to the
SGRC within 30 days of the decision of the DGRC, which shall take a decision
within 30 days of receipt of appeal.
Step II- If either of the parties is not satisfied with the decision, they can go to
the NGRC within 30 days of the decision of the SGRC, which shall take a decision
within 30 days of receipt of appeal. The decision of NGRC shall be final.
C. Grievance of insurance company
i) Grievance against district authorities/ health care provider
If Insurance Company has a grievance against District Authority / Health Care
Provider or an agency of the State Government, it can approach the SGRC for
resolution. The SGRC shall decide the matter within 30 days of the receipt of the
grievance.
In case of dissatisfaction with the decision of the SGRC, the affected party can file
an appeal before NGRC within 30 days of the decision of the SGRC and NGRC
shall take a decision within 30 days of the receipt of appeal after seeking a report
from the other party. The decision of NGRC shall be final.
1.2. Functions of Grievance Redressal Committees
A. Functions of the DGRC:
The DGRC shall perform all functions related to handling and resolution of grievances
within their respective Districts. The specific functions will include:
i) Review grievance records.
ii) Call for additional information as required either directly from the
Complainant or from the concerned agencies which could be the Insurer or
an EHCP or the SHA or any other agency/ individual directly or indirectly
associated with the Scheme.
iii) Conduct grievance redressal proceedings as required.
iv) If required, call for hearings and representations from the parties concerned
while determining the merits and demerits of a case.
v) Adjudicate and issue final orders on grievances.
vi) In case of grievances that need urgent redressal, develop internal
mechanisms for redressing the grievances within the shortest possible time,
which could include but not be limited to convening special meetings of the
Committee.
vii) Monitor the grievance database to ensure that all grievances are resolved
within 30 days.
B. Functions of the SGRC:
The SGRC shall perform all functions related to handling and resolution of all
grievances received either directly or escalated through the DGRC. The specific
functions will include:
i) Oversee grievance redressal functions of the DGRC including but not limited
to monitoring the turnaround time for grievance redressal.
ii) Act as an Appellate Authority for appealing against the orders of the DGRC.
iii) Perform all tasks necessary to decide on all such appeals within 30 days of
receiving such appeal.
iv) Adjudicate and issue final orders on grievances.
v) Nominate District Grievance Officer (DGO) at each District.
vi) Direct the concerned Insurance Company to appoint District Nodal Officer of
each district.
C. Functions of the NGRC:
The NGRC shall act as the final Appellate Authority at the National level.
i) The NGRC shall only accept appeals against the orders of the SGRC of a State.
ii) The decision of NGRC will be final.
1.3. Lodging of Grievances/ Complaints
A. If any stakeholder has a complaint (complainant) against any other stakeholder
during the subsistence of the Policy Cover Period or thereafter, in connection with
the validity, interpretation, implementation or alleged breach of the Insurance
Contract between the Insurer and the SHA or a Policy or of the terms of their
agreement (for example, the Services Agreement between the Insurer and an
Empanelled Health Care Provider), then such complainant may lodge a complaint by
online grievance redressal portal or letter or e-mail.
B. For this purpose, a stakeholder includes: any PMRSSM Beneficiary; an empanelled
health care provider (EHCP); a De-empanelled Health Care Provider; the Insurer or
its employees; the SHA or its employees or nominated functionaries for
implementation of the Scheme (DNOs, State Nodal Officer, etc.); and any other
person having an interest or participating in the implementation of the Scheme or
entitled to benefits under the PMRSSM Cover.
C. A complainant may lodge a complaint in the following manner:
i) directly with the DGNO of the district where such stakeholder is located or
where such complaint has arisen and if the stakeholder is located outside the
Service Area, then with any DGNO located in the Service Area; or
ii) with the SHA: If a complaint has been lodged with the SHA, they shall forward such complaint to the concerned DGNO.
D. Upon a complaint being received by the DGNO, the DGNO shall decide whether the
substance of the complaint is a matter that can be addressed by the stakeholder
against whom the complaint is lodged or whether such matter requires to be dealt
with under the grievance redressal mechanism.
E. If the DGNO decides that the complaint must be dealt with under the grievance
redressal mechanism, the DGNO shall refer such complaint to the Convener of the
relevant Grievance Redressal Committee.
F. If the DGNO decides that the complaint need not be dealt with under the grievance
redressal mechanism, then the procedures set out in various process/guidelines
shall apply.
1.4. Redressal of Complaints
A. The DGNO shall enter the particulars of the complaint on the Web-based Central
Complaints and Grievance Management System (CCGMS) established by the
MoHFW.
B. The CCGMS will automatically: (i) generate a Unique Complaint Number (UCN); (ii)
categorize the nature of the complaint; and (iii) an e-mail or letter to be sent to the
appropriate stakeholder to which such category of complaint is to be referred
(including updating on phone).
C. Once the UCN is generated, the DGNO shall send or cause to be sent an
acknowledgement email/phone call to the complainant and provide the complainant
with the UCN. Upon receipt of the UCN, the complainant will have the ability to
track the progress of complaint resolution online through CCGMS and use the same
at the time of calling the helpline for allowing easy retrieval of the specific complaint
data.
D. The stakeholder against whom a complaint has been lodged must send its
comments/ response to the complainant and copy to the DGNO within 15 days. If
the complaint is not addressed within such 15-day period, the DGNO shall send a
reminder to such stakeholder for redressal within a time period specified by the
DGNO.
E. If the DGNO is satisfied that the comments/ response received from the stakeholder
will addresses the complaint, then the DGNO shall communicate this to the
complainant by e-mail and update the CCGMS.
F. If the DGNO is not satisfied with the comments/ response received or if no
comments/ response are received from the stakeholder despite a reminder, then
the DGNO shall refer such complaint to the Convener of the relevant Grievance
Redressal Committee depending on the nature of the complaint after which the
procedures set out shall apply.
1.5. Grievance Redressal Mechanism
Upon escalation of a complaint for grievance redressal the following procedures
shall apply:
A. The DGNO/SGRC shall update the CCGMS to change the status of the complaint to a
grievance, after which the CCGMS shall categorize the grievance and automatically
refer it to the Convenor of the relevant Grievance Redressal Committee by way of email.
B. The Convenor of the relevant Grievance Redressal Committee shall place the
grievance before the Grievance Redressal Committee for its decision at its next
meeting.
C. Each grievance shall be addressed by the relevant Grievance Redressal Committee
within a period of 30 days of receipt of the grievance. For this purpose, each
Grievance Redressal Committee shall be convened at least once every 30 days to
ensure that all grievances are addressed within this time frame. Depending on the
urgency of the case, the Grievance Redressal Committee may decide to meet earlier
for a speedier resolution of the grievance.
D. The relevant Grievance Redressal Committee shall arrive at a reasoned decision
within 30 days of receipt of the grievance. The decision of the relevant Grievance
Redressal Committee shall be taken by majority vote of its members present. Such
decision shall be given after following the principles of natural justice, including
giving the parties a reasonable opportunity to be heard
E. If any party to a grievance is not satisfied with the decision of the relevant Grievance
Redressal Committee, it may appeal against the decision within 30 days to the
relevant Grievance Redressal Committee or other authority having powers of
appeal.
F. If an appeal is not filed within such 30-day period, the decision of the original
Grievance Redressal Committee shall be final and binding.
G. A Grievance Redressal Committee or other authority having powers of appeal shall
dispose of an appeal within 30 days of receipt of the appeal. The decision of the
Grievance Redressal Committee or other authority with powers of appeal shall be
taken by majority vote of its members. Such decision shall be given after following
the principles of natural justice, including giving the parties a reasonable opportunity
to be heard. The decision of the Grievance Redressal Committee or other authority
having powers of appeal shall be final and binding.
1.6. Proceedings initiated by the State Health Authority, State Grievance Redressal
Committee, the National Health Authority
The SHA, SGRC and/ or the National Health Authority (NHA) shall have the standing to
initiate suo moto proceedings and to file a complaint on behalf of itself and PMRSSM
Beneficiaries under the Scheme.
A. Compliance with the Orders of the Grievance Redressal Committees
i) The Insurer shall ensure that all orders of the Grievance Redressal
Committees by which it is bound are complied with within 30 days of the
issuance of the order, unless such order has been stayed on appeal.
ii) If the Insurer fails to comply with the order of any Grievance Redressal
Committee within such 30-day period, the Insurer shall be liable to pay a
penalty of Rs. 25,000 per month for the first month of such non-compliance
and Rs. 50,000 per month thereafter until the order of such Grievance
Redressal Committee is complied with. The Insurer shall be liable to pay such
penalty to the SHA within 15 days of receiving a written notice.
iii) On failure to pay such penalty, the Insurer shall incur an additional interest at
the rate of one percent of the total outstanding penalty amount for every
15 days for which such penalty amount remains unpaid.
B. Complaints/ Suggestions received through Social Media/Call centre
As Social Media channels will be handled by NHA, hence, the complaints/
suggestions raised through Social Media channels like, Facebook, twitter handles,
etc. will be routed to the respective SGNO by NGNO (National Grievance Nodal
Officer). SGNO needs to register the same on the Grievance portal and publish a
monthly report on the action taken to the NGNO.
Complaint may also be lodged through Call center by beneficiary. Call center
need to register the details like complaint details in the defined format and
forward the same to State Grievance Nodal Officer of the State concerned.
SGNO needs to upload the details of the complaint on the grievance portal and
allocate the same to the concerned District. The Complaint / grievance will be
redressed as per guidelines.
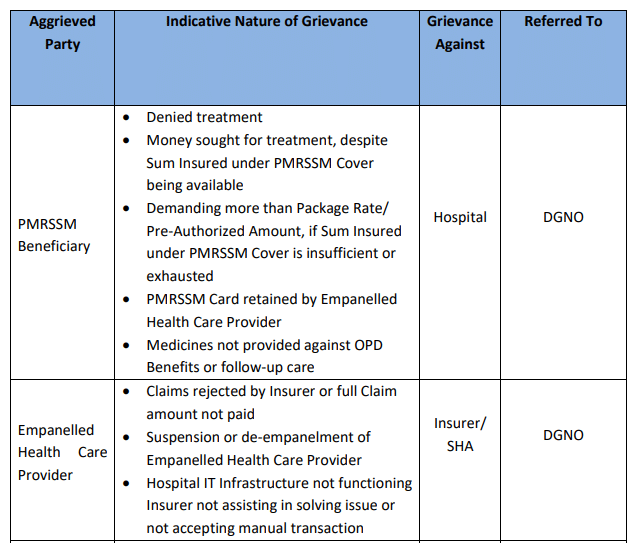
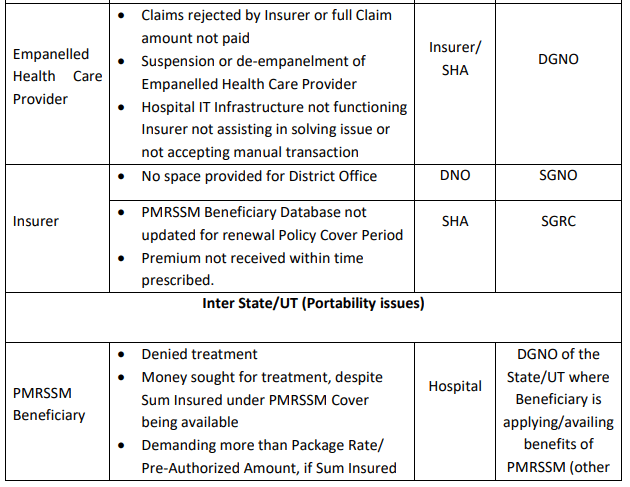
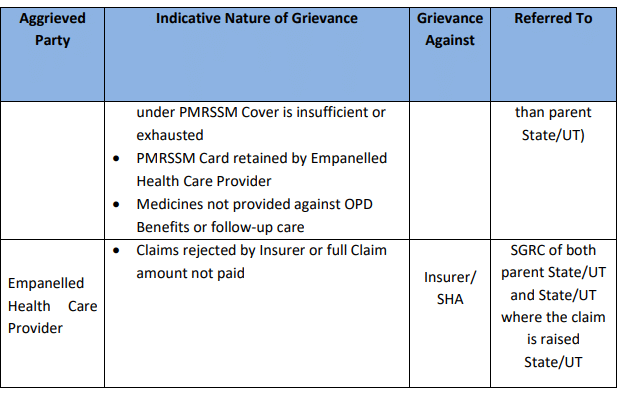
Note: Matrix for grievance referral under the Scheme is presented in the table below:
Related Post on Ayushman Bharat | PM – Jan Arogya Yojana
Free Study Material on PM – Jan Arogya Yojana
Check Am I Eligible for Ayushman Bharat | PM – Jan Arogya Yojana
Ayushman Bharat : Policy & Guidelines : PM-JAY
Ayushman Mitra : Guidelines under PM-JAY
Ayushman Bharat : Annexure-1 PreAuthorization Form :Download /Print
Ayushman Bharat : Annexure II – Discharge Summary : Download /Print
Website mera.pmjay.gov.in for Ayushman Bharat
Ayushman Bharat launched by PM on 23.09.2018; PMJAY at Ranchi
Ayushman Bharat Yojana :Pradhan Mantri Jan Aarogya Yojana Features :
Use of Aadhaar in Ayushman Bharat – Desirable and not “Must”
Ayushman Bharat – National Health Protection Mission : Features


